- Federal Cuts to Health Care
- State Budget and Health Care Financing
- Strong Partnerships Protect Patient Care
- Hospital Financial Challenges
- Optimizing Medicaid
- Hospitals 101
- Rural Health
- Additional Issues
- 340B
- End-of-Life Options Act Materials
- Hospital Community Benefit
- Facility Fees
- Hospital Discounted Care
- Hospital Rate-Setting
- Hospital Workforce
- How Hospitals Get Paid
- Improve Insurance Processes
- Medicaid Enrollment
- Medicaid RAC Audits
- Responsibly Modernizing Medical Liability Caps
- Save Our Safety Net
Improving Insurance Processes for Patients in Colorado
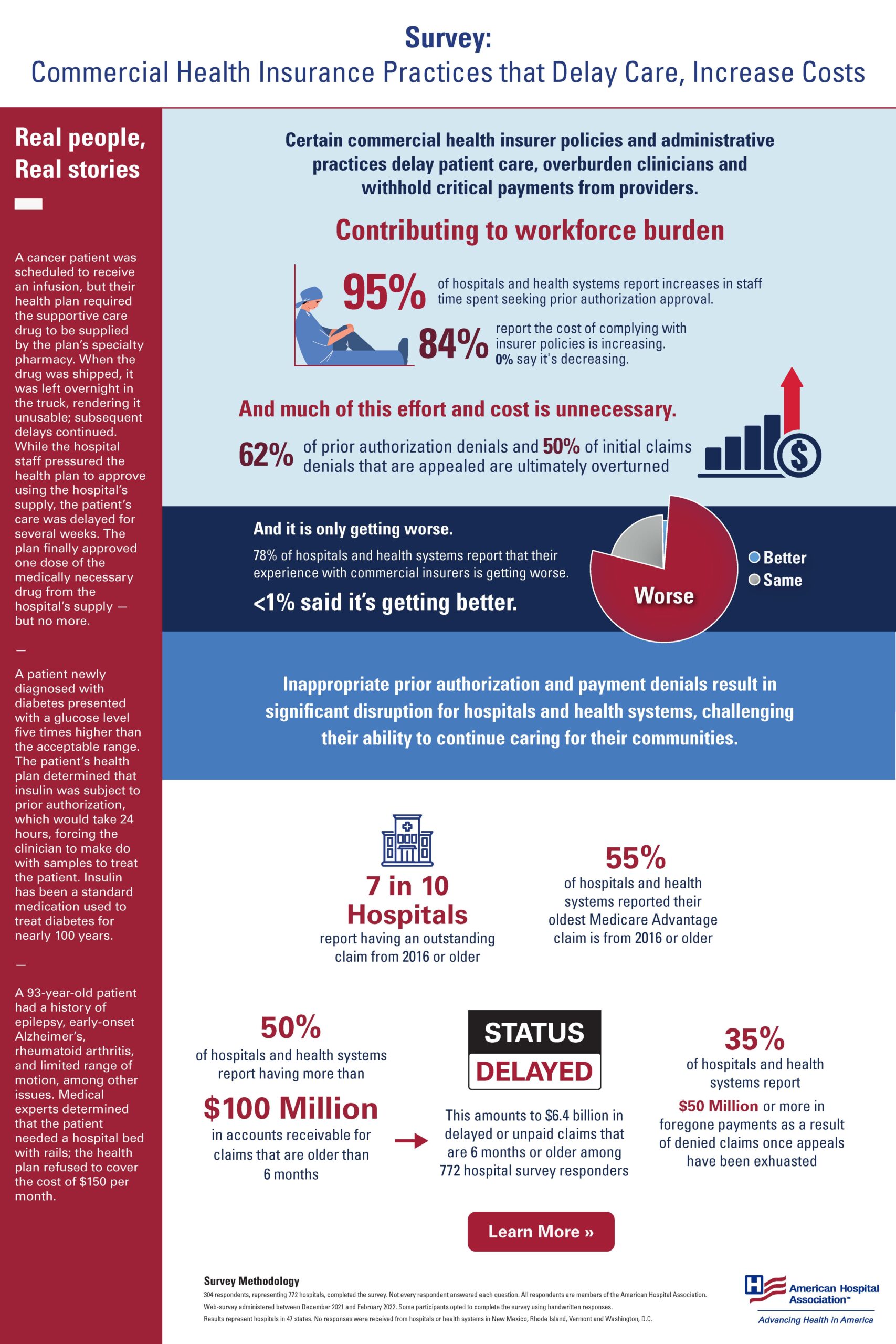
What You Need to Know:
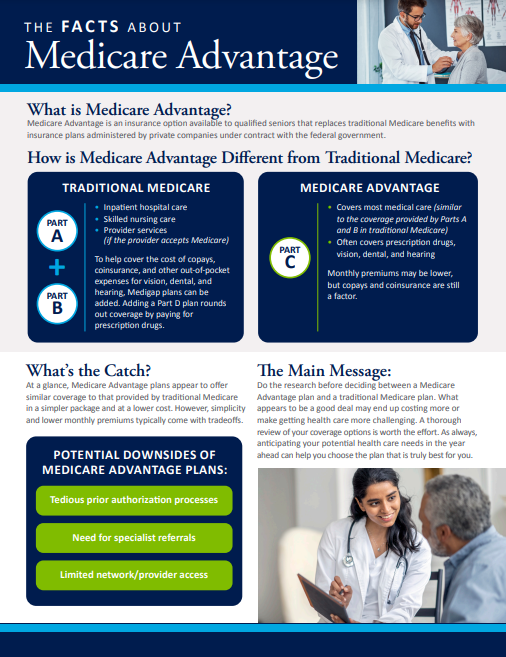
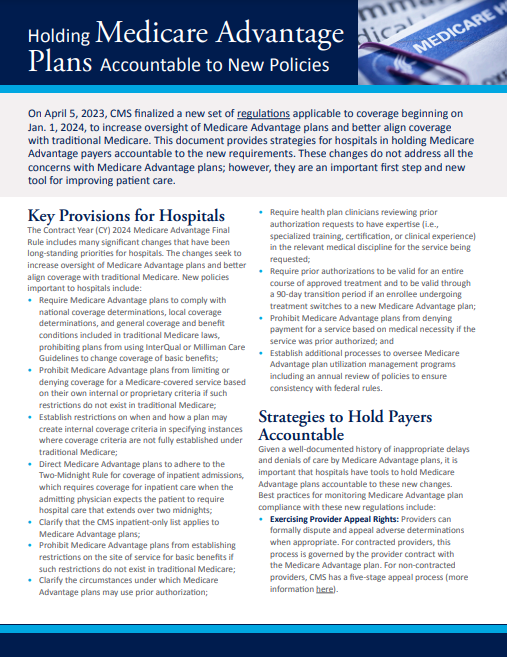
Our patients rely upon a functional and collaborative relationship between providers (clinicians and hospitals) and third-party payers (insurance companies) to ensure that they can receive essential health care services in a timely manner. Health insurance companies are making it harder all the time for hospitals to get paid for care that is necessary, and in many cases, that was already authorized and provided to patients. This adds significant delays and unnecessary costs to the health care system.
Colorado Hospital Perspective:
In a survey of CHA member hospitals and health systems, more than 90 percent of respondents said insurance company issues are significant and getting worse. Due to recent changes by insurance companies, hospitals invest significant resources to manage health insurer requirements, diverting staff and time away from patient care. For examples:
- Colorado hospitals report findings similar to a national study by the American Hospital Association (AHA), which found that 95 percent of hospital report increases in staff time seeking prior authorization approval.
- Additional requirements add unnecessary cost to the system. In the same AHA survey, 84 percent of hospitals said the cost of complying with insurer policies is increasing.
- Carriers are not paying when services are provided to patients. Fifteen percent of all first claims are denied, and 57 percent of initial claims denials that are appeals are ultimately overturned.
Taking Action:
In 2024, CHA joined a coalition of other health care providers to create and pass legislation to fix some of the many prior authorization challenges used by insurance companies. The Health Can’t Wait Colorado coalition supported House Bill 24-1149, which will require that insurance companies eliminate or modify onerous prior authorization requirements.